States Best and Least Prepared for the Coronavirus Pandemic
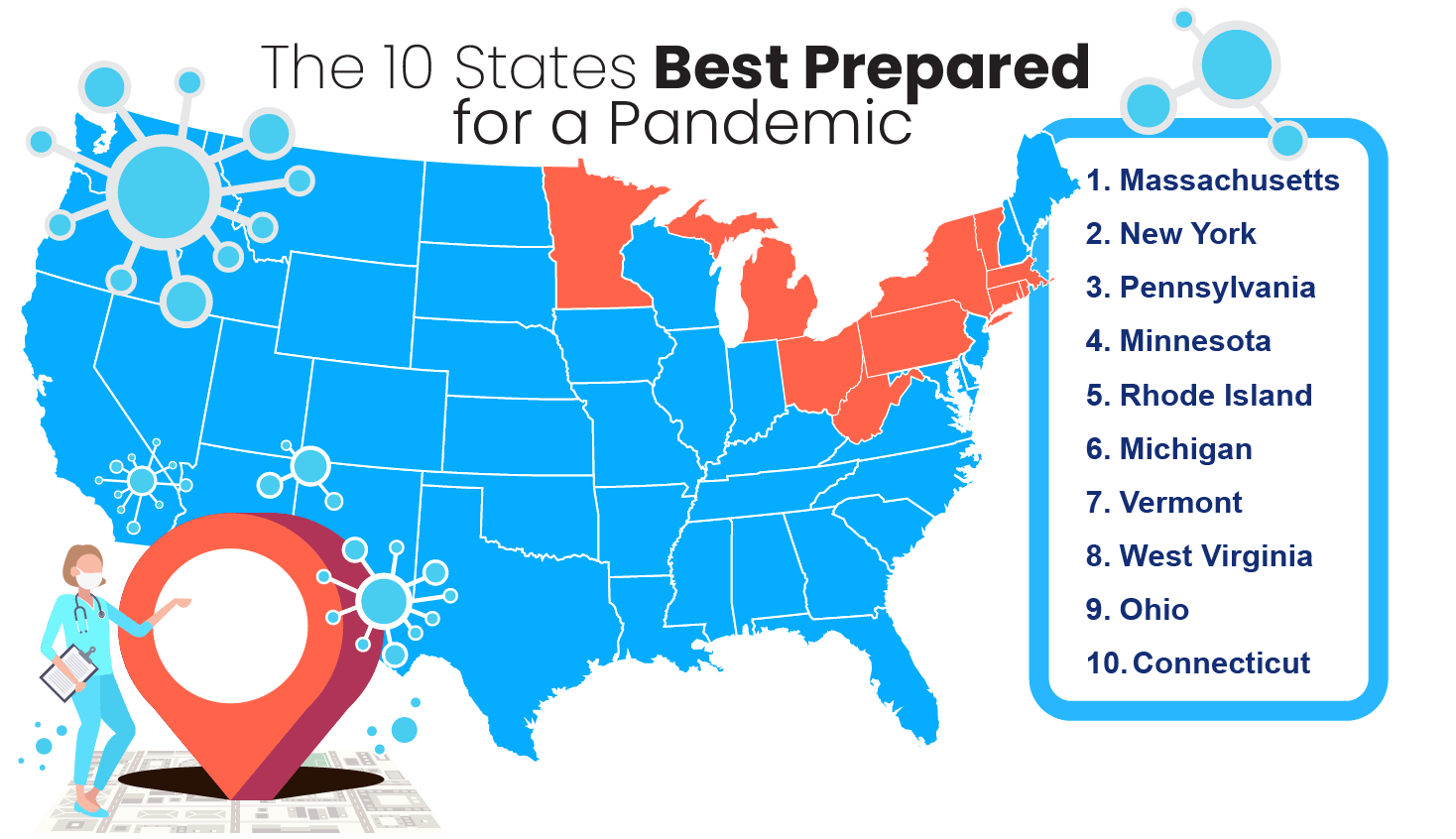
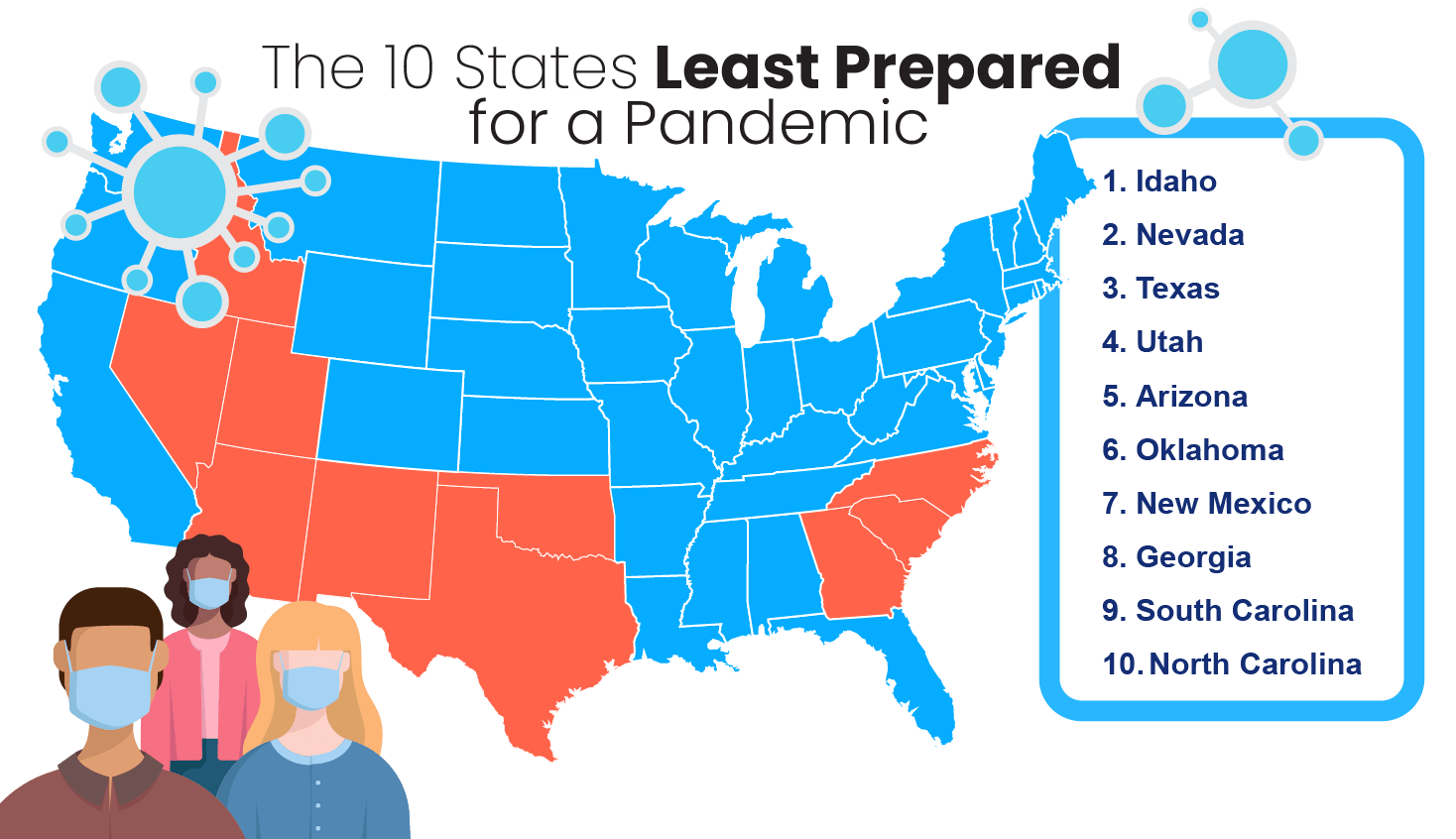
In our list of the states best and least prepared for the coronavirus pandemic, Massachusetts, New York, and Pennsylvania came out on top. Each of the three most prepared states managed to have under 7 percent of its population uninsured. Idaho, Nevada, and Texas were the states least prepared for COVID-19 — all having uninsured residents making up at least 12 percent of their total population.
Read moreReady to compare quick life insurance quotes?
Your life insurance quotes are always free.
Secured with SHA-256 Encryption
Laura D. Adams
Insurance & Finance Analyst
Laura Adams is one of the nation’s leading finance, insurance, and small business authorities. As an award-winning author, spokesperson, and host of the top-rated Money Girl podcast since 2008, millions of readers and listeners benefit from her practical advice. Her mission is to empower consumers to live healthy and rich lives by planning for the future and making smart money decisions. She rec...
Insurance & Finance Analyst
UPDATED: Jan 10, 2025
It’s all about you. We want to help you make the right life insurance coverage choices.
Advertiser Disclosure: We strive to help you make confident life insurance decisions. Comparison shopping should be easy. We are not affiliated with any one life insurance company and cannot guarantee quotes from any single company.
Our life insurance industry partnerships don’t influence our content. Our opinions are our own. To compare quotes from many different life insurance companies please enter your ZIP code above to use the free quote tool. The more quotes you compare, the more chances to save.
Editorial Guidelines: We are a free online resource for anyone interested in learning more about life insurance. Our goal is to be an objective, third-party resource for everything life insurance-related. We update our site regularly, and all content is reviewed by life insurance experts.
UPDATED: Jan 10, 2025
It’s all about you. We want to help you make the right life insurance coverage choices.
Advertiser Disclosure: We strive to help you make confident life insurance decisions. Comparison shopping should be easy. We are not affiliated with any one life insurance company and cannot guarantee quotes from any single company.
Our life insurance industry partnerships don’t influence our content. Our opinions are our own. To compare quotes from many different life insurance companies please enter your ZIP code above to use the free quote tool. The more quotes you compare, the more chances to save.
On This Page
Here’s What You Need to Know:
- States with a lot of doctors, hospital beds, and insured residents are best prepared to face a pandemic
- The states best prepared to face a pandemic are concentrated in the Northeastern United States
- States with a wide urban-rural divide face larger challenges in preparing for public health emergencies
It’s true: The coronavirus and pandemic preparedness in general is on all our minds these days.
The number of COVID-19 cases in the United States is nearly 1 million. And devastatingly, the number of COVID-19 deaths is already well over 30,000.
This article will examine the states best and least prepared for the coronavirus pandemic because readiness is crucial for states to protect and treat their residents if the infection rate continues to rise.
There is also a chance that the coronavirus will have widespread and unknown effects. For instance, people are nervously monitoring if their life insurance covers coronavirus.
For those who are worried, in many cases, life insurance companies will cover coronavirus. One type of policy that insurers may issue for those wanting financial protection during the coronavirus pandemic is called term life insurance.
Use our FREE online tool to find the best insurance policies for you based on your location and demographic information.
In a larger view, our researchers became interested in investigating what states were best prepared to meet a pandemic such as COVID-19 head-on. However, it was also important to us to make sure this feature laid out the state-by-state preparedness for any pandemic or other major events that would require widespread medical action.
In this study, we determined which 10 states were the best prepared for the coronavirus pandemic and which were the least prepared.
Additionally, we will discuss the cities with the best hospitals and medical schools, and cities where research on the coronavirus and other infectious diseases is at the innovation forefront.
In the frequently asked questions section, we’ll go over the coronavirus pandemic more broadly. Some of the topics or questions we’ll answer are:
- When will there be a coronavirus vaccine?
- COVID-19 vaccine progress
- CDC guidelines for COVID-19
- What is COVID-19?
- COVID-19 news
We know this time is scary. But the more knowledge we all have, the better prepared we are — physically, emotionally, and financially — to deal with an ongoing crisis.
Read on to find out how prepared your state is to face the coronavirus or any public health crisis that may come our way.
The 10 States Best Prepared for a Pandemic
Public health initiatives and infrastructure is largely a state-by-state issue in the United States. And not all states are created equal.
We based our state-by-state preparedness for pandemic rankings based on three factors: Number of hospital beds per 1,000 residents, number of active physicians per 100,000 residents, and percent of uninsured residents.
In the table below, you can find our rankings, best prepared to worst prepared, for states and their preparedness to combat a pandemic such as the current coronavirus outbreak
State Pandemic Readiness Scoring
State Hospital Beds
(per 1k ppl)Active Physicians
(per 100k ppl)Uninsured
ResidentsPreparedness
Rank
Alabama 3.1 217 11.00% 35
Alaska 2.2 277 14.80% 40
Arizona 1.9 242 12.10% 46
Arkansas 3.2 208 9.30% 30
California 1.8 280 8.20% 34
Colorado 1.9 286 8.70% 31
Connecticut 2 352 6.30% 10
Delaware 2.2 285 6.10% 11
Florida 2.6 265 16.00% 36
Georgia 2.4 229 15.50% 43
Hawaii 1.9 314 4.60% 12
Idaho 1.9 193 11.80% 50
Illinois 2.5 284 7.90% 17
Indiana 2.7 231 9.60% 32
Iowa 3 218 5.50% 16
Kansas 3.3 228 10.10% 28
Kentucky 3.2 231 6.40% 13
Louisiana 3.3 260 9.60% 18
Maine 2.5 330 10.20% 19
Maryland 1.9 386 7.00% 14
Massachusetts 2.3 450 3.30% 1
Michigan 2.5 287 6.10% 6
Minnesota 2.5 303 5.10% 4
Mississippi 4 191 14.50% 39
Missouri 3.1 273 10.90% 25
Montana 3.3 247 10.40% 26
Nebraska 3.6 239 9.60% 22
Nevada 2.1 214 13.10% 49
New Hampshire 2.1 315 7.00% 20
New Jersey 2.4 307 9.00% 21
New Mexico 1.8 245 11.00% 44
New York 2.7 375 6.60% 2
North Carolina 2.1 255 12.60% 41
North Dakota 4.3 238 8.60% 15
Ohio 2.8 293 7.10% 9
Oklahoma 2.8 207 16.50% 45
Oregon 1.6 303 8.20% 33
Pennsylvania 2.9 321 6.60% 3
Rhode Island 2.1 370 5.40% 5
South Carolina 2.4 230 13.10% 42
South Dakota 4.8 240 10.80% 24
Tennessee 2.9 253 11.30% 29
Texas 2.3 225 19.40% 48
Utah 1.8 216 10.00% 47
Vermont 2.1 367 5.50% 7
Virginia 2.1 263 10.20% 37
Washington 1.7 279 7.10% 27
West Virginia 3.8 263 7.50% 8
Wisconsin 2.1 265 6.40% 23
Wyoming 3.5 208 14.20% 38
Read more: Missouri Life Insurance
As you can see, states in the densely-populated Northeast corridor reign supreme when it comes to pandemic preparedness. By and large, these states are prepared for a public health crisis like COVID-19 because they have a high share of available hospital beds and actively practicing doctors plus a low share of residents without health insurance.
So let’s take a closer look at these well-prepared states and what makes them most ready to face a pandemic like the coronavirus or the next public health crisis that may come our way.
#1 – Massachusetts
The Commonwealth of Massachusetts earns the top spot on our list of states best prepared to meet the coronavirus pandemic head-on.
With the lowest percentage of uninsured residents and the highest number of doctors per capita, the Bay State is leaps and bounds ahead of almost any other state in the country when it comes to health care in general.
Health Care in Massachusetts
| Population | Hospital Beds (per 1k ppl) | Active Physicians (per 100k ppl) | Uninsured Residents |
|---|---|---|---|
| 6.893 million | 2.3 | 449.5 | 3.3% |
In fact, Massachusetts’s largest city and capital, Boston, is ranked the No. 2 city for health care overall (after Tokyo, Japan) of any city in the world.
Massachusetts is home to not only the best hospital in the United States but also the best medical school: Harvard University School of Medicine. During the coronavirus pandemic, professors and medical students from Harvard are filming helpful videos such as the one below to help educate us on thriving during this difficult time.
But even a state like Massachusetts has its health care problems. Given the concentration of medical institutions in the eastern part of the state in and around Boston, Western Massachusetts and particularly Berkshire County can sometimes seem like a health care desert, with few hospitals and overbooked medical professionals trying to meet the needs of their communities.
#2 – New York
New York City is currently the epicenter of the coronavirus pandemic, with more cases and more deaths than any other city in the United States. That’s why you can see such a big dark circle in and around New York City on the map at the top of this feature, with constantly updated data from Johns Hopkins University.
But in reality, New York is well-prepared in many ways for such a public health crisis, with a high number of doctors per capita and a relatively low number of uninsured residents.
Health Care in New York
| Population | Hospital Beds (per 1k ppl) | Active Physicians (per 100k ppl) | Uninsured Residents |
|---|---|---|---|
| 19.45 million | 2.7 | 375.1 | 6.6% |
Like Massachusetts, New York is home to many of the finest hospitals and medical schools in the country, such as the Grossman School at New York University and the Columbia University School of Medicine.
But also like Massachusetts, these institutions are overly concentrated in the New York City metropolitan area. This leaves much of upstate New York, where more than half of the state’s population lives, less prepared than the New York City region itself.
#3 – Pennsylvania
With two powerhouse cities for medical care — Philadelphia in the east and Pittsburgh in the west — the Commonwealth of Pennsylvania has an especially high number of doctors per capita.
Health Care in Pennsylvania
| Population | Hospital Beds (per 1k ppl) | Active Physicians (per 100k ppl) | Uninsured Residents |
|---|---|---|---|
| 12.8 million | 2.9 | 320.5 | 6.6% |
Children’s Hospital of Pittsburgh of UPMC is one of the leading children’s hospitals in the United States, with a beautiful campus located in the Steel City’s Lawrenceville neighborhood. In the video below, you can get a tour of this state-of-the-art facility.
In a state as physically large as Pennsylvania, however, hospital beds are not spread evenly among the population.
The state’s biggest medical centers can be found in Pittsburgh and Philadelphia, leaving much of the state struggling to build and staff hospitals to deal with emergencies, both everyday and pandemic-related.
#4 – Minnesota
Residents of Minnesota are lucky to have one of the best departments of health in the country, as well as one of the top medical institutions, the Mayo Clinic. The Land of 10,000 Lakes is also home to a lot of doctors per capita and relatively few uninsured residents.
Health Care in Minnesota
| Population | Hospital Beds (per 1k ppl) | Active Physicians (per 100k ppl) | Uninsured Residents |
|---|---|---|---|
| 5.64 million | 2.5 | 302.7 | 5.1% |
As is the case in many other large states, Minnesota has an over-concentration of health care options in the Twin Cities area, and a lack of options in many rural areas of the state. But this isn’t a problem unique to Minnesota. Rural health care is a problem across the United States.
According to the Rural Health Information Hub, home health, hospice and palliative care, mental health, substance abuse, obstetric, and oral health services are especially difficult to access in rural areas.
Read about Minnesota life insurance policies to protect yourself for a pandemic or major illness.
#5 – Rhode Island
The Ocean State, which is physically the smallest state in the United States, has some of the best health care options you’ll find anywhere. An outsized number of doctors per capita call Rhode Island home.
Health Care in Rhode Island
| Population | Hospital Beds (per 1k ppl) | Active Physicians (per 100k ppl) | Uninsured Residents |
|---|---|---|---|
| 1.059 million | 2.1 | 370 | 5.4% |
Unlike a lot of states on this list, Rhode Island has relatively few actual rural areas, meaning the state’s population mostly has easy physical access to medical facilities, especially in Providence, home of the Brown University School of Medicine.
Additionally, Rhode Island is taking big steps to make sure its residents are protected during this frightening time. HealthSourceRI, the state’s official public health care marketplace, has extended the open enrollment period for health insurance coverage under the current coronavirus pandemic.
#6 – Michigan
Residents of the Great Lake State have a fairly low uninsured rate and access to some world-class medical institutions, especially those connected to the flagship University of Michigan campus in Ann Arbor.
Health Care in Michigan
| Population | Hospital Beds (per 1k ppl) | Active Physicians (per 100k ppl) | Uninsured Residents |
|---|---|---|---|
| 9.987 million | 2.5 | 287 | 6.1% |
But conditions across the state of Michigan itself are not equal. For instance, many hospitals in Detroit are underfunded and struggling to keep up healthy conditions during the coronavirus pandemic. You can see disturbing evidence of this in the video below focusing on Detroit Medical Center’s Sinai-Grace Hospital.
As one anonymous hospital employee explains, “The funeral homes are full. The morgues are full. It’s just so unsanitary [inside the hospital].” So while health care options in wealthier cities like Ann Arbor, home of the University of Michigan, propel the state to the top of our list, conditions are not equal everywhere.
Related: Michigan Life Insurance
#7 – Vermont
One of the least populated states in the United States, Vermont, perhaps surprisingly, finds itself well-prepared to face a pandemic. The Green Mountain State has a low share of uninsured residents and a high number of doctors per capita.
Health Care in Vermont
| Population | Hospital Beds (per 1k ppl) | Active Physicians (per 100k ppl) | Uninsured Residents |
|---|---|---|---|
| 623,989 | 2.1 | 367.1 | 5.5% |
With one of the finest medical schools at a public university located in Burlington at the University of Vermont, the state is well-prepared to meet the coronavirus pandemic and other similar public health crises.
On average, the state of Vermont spends over $10,000 in public money a year on each resident’s health care. Only Alaska, Massachusetts, and Delaware spend more on health care expenditures per capita, according to the Kaiser Family Foundation.
#8 – West Virginia
Many folks might be surprised to see West Virginia ranked as one of the 10 states best prepared to face a pandemic. But with 3.8 hospital beds per 1,000 residents, Wild West Virginia has more hospital beds per capita than 94 percent of all the other states across the country.
Health Care in West Virginia
| Population | Hospital Beds (per 1k ppl) | Active Physicians (per 100k ppl) | Uninsured Residents |
|---|---|---|---|
| 1.792 million | 3.8 | 263.4 | 7.5% |
As you can see in the video below from PBS News Hour, West Virginia chose to expand Medicaid under the Affordable Care Act, which brought medical care to a large swath of the state’s primarily rural population.
In 2010, 21 percent of West Virginians were uninsured. With the adoption of Medicaid expansion, the percentage of uninsured residents fell to 9 percent by 2015 and today is even lower, at 7.5 percent. That’s great news for West Virginians, and a model other mostly rural states across the country might look to in protecting their residents.
From Wheeling to Morgantown, a variety of West Virginia life insurance policies are available to help protect you and your family in the case of a tragedy.
#9 – Ohio
Given the number of large cities in Ohio — especially Cleveland, Cincinnati, and Columbus — residents of the state mostly live within relatively close proximity to solidly-ranked and prepared hospital centers, places that are well-prepared to treat those who test positive for the coronavirus.
Health Care in Ohio
| Population | Hospital Beds (per 1k ppl) | Active Physicians (per 100k ppl) | Uninsured Residents |
|---|---|---|---|
| 11.69 million | 2.8 | 292.7 | 7.1% |
The Buckeye State is also home to one of the nation’s top hospitals, the Cleveland Clinic, which is well-regarded for its cardiovascular health programs. The Cleveland Clinic includes 18 hospitals with 6,026 hospital beds, and they have 9.75 million patient visits every year.
While the United States average for health care expenditures per capita by state of residence Is $8,045 per year, Ohio is spending a bit more than average, putting $8,712 into each resident’s health care.
#10 – Connecticut
Rounding out our list of the 10 best-prepared states to face a pandemic is another Northeastern state, Connecticut. The Constitution State has an especially high number of active physicians per capita.
Health Care in Connecticut
| Population | Hospital Beds (per 1k ppl) | Active Physicians (per 100k ppl) | Uninsured Residents |
|---|---|---|---|
| 3.565 million | 2.0 | 352.1 | 6.3% |
Connecticut is not always at the forefront of the public’s mind in comparison to its high-brow neighbors New York and Massachusetts, but Yale, located in New Haven, is one of the most innovative universities in the United States. During the coronavirus pandemic, doctors, researchers, and medical students at the Yale School of Medicine are filming some helpful videos to keep us all in the know.
This video provides a fun and useful illustrated summary of the actual science behind COVID-19. With so much false and misinformed information being passed around social media sites like Facebook and Twitter right now about the pandemic, it’s important to turn to trusted and reputable sources such as Yale or the Centers for Disease Control and Prevention for the best and safest information possible.
Sadly, a pandemic is a time that reminds us to learn as much as we can about the types of life insurance available to us and our families. Educate yourself about Connecticut life insurance in our guide.
Your life insurance quotes are always free.
Secured with SHA-256 Encryption
The 10 States Least Prepared for a Pandemic
Conversely, not all states are well prepared for a pandemic such as the COVID-19 health crisis.
As with our list of best-prepared states above, we considered a variety of telling health care infrastructure factors that put certain states at a higher risk when it comes to public health events such as the coronavirus outbreak.
Some of these states have a low number of hospital beds or active physicians per capita. And some have a high percentage of uninsured residents. This is an important factor to consider because uninsured people are less likely to seek medical treatment, even if they show signs of having a highly contagious virus like the coronavirus.
According to the federal government’s HealthyPeople.gov, access to health care is key to a variety of wellness indicators, including:
- Overall physical, social, and mental health status
- Disease prevention
- Detection, diagnosis, and treatment of illness
- Quality of life
- Preventable death
- Life expectancy
Without easy and proven access to regular medical care for all residents, a state is bound to be less prepared to face a public health crisis than they could or should be.
In many of the states below, the urban-rural divide is especially prominent and helps propel these states to the least prepared list in the first place.
Access to health care in rural areas is a pressing public health issue. According to the Rural Health Information Hub, barriers to health care in rural areas include distance and transportation, lack of health insurance coverage, poor health literacy, social stigma, privacy issues, and workforce shortages.
Let’s take a closer look at the 10 states we’ve ranked as least prepared to face a pandemic such as the COVID-19 crisis.
#1 – Idaho
Bottom line: Idaho faces a shortage of doctors. With only one medical school, the Idaho College of Osteopathic Medicine at Idaho State University, which only opened in 2016, most doctors in Idaho have to be recruited from other states.
Health Care in Idaho
| Population | Hospital Beds (per 1k ppl) | Active Physicians (per 100k ppl) | Uninsured Residents |
|---|---|---|---|
| 1.787 million | 1.9 | 192.6 | 11.8% |
Idaho is also a fairly large physical state with only one city, Boise, with over 200,000 residents. Largely rural states, which comprise the majority of this least prepared list, face bigger challenges in meeting the health care needs of their population.
Finally, Idaho spends relatively little on health care per capita each year. While the United States average for health care expenditures per capita by state of residence Is $8,045 per year, Idaho spends only $6,927.
Learn about Idaho life insurance policies to do your part in planning ahead.
#2 – Nevada
Like its northern neighbor Idaho, the state of Nevada is a geographically large state with a majority of the population centered in two locations. Over 90 percent of Nevadians live in either the Las Vegas or Reno metropolitan statistical areas, which makes giving medical access to those in rural areas an especially challenging problem.
Health Care in Nevada
| Population | Hospital Beds (per 1k ppl) | Active Physicians (per 100k ppl) | Uninsured Residents |
|---|---|---|---|
| 3.08 million | 2.1 | 213.5 | 13.1% |
As you can see in the video below from KSNV News 3 Las Vegas, the state of Nevada is attempting to meet its challenging health care needs by continually expanding on the Affordable Care Act. Like many other states, Nevada has extended its open enrollment period to meet the special circumstances the COVID-19 crisis has created.
With over 13 percent of the population still without health insurance, Nevada has some catching up to do. Learn more about another type of important insurance, term life insurance, in our comprehensive Nevada life insurance guide.
Read More : The Top (and Bottom) 10 states for term life insurance
#3 – Texas
With over 19 percent of Texans lacking health insurance, the Lone Star State has more uninsured residents than any other state in the United States. Those without health insurance are far less likely to seek medical treatment, even if they are showing symptoms of a virus as dangerous and contagious as COVID-19.
Health Care in Texas
| Population | Hospital Beds (per 1k ppl) | Active Physicians (per 100k ppl) | Uninsured Residents |
|---|---|---|---|
| 29 million | 2.3 | 224.8 | 19.4% |
One bright spot to consider for Texas: The state has 12 medical schools. This means that the state is continuing to train more doctors than almost any other place in the United States.
For better and for worse, Texas is a gigantic state. The Lone Star State covers 268,597 square miles, which means many Texans live far away from the state’s large cities, such as Austin, Dallas, El Paso, Fort Worth, Houston, and San Antonio.
The National Academies Press defines health care access as:
“The timely use of personal health services to achieve the best possible health outcomes.”
With so many residents living far away from well-stocked and prepared medical centers, Texas certainly has a health care access problem.
#4 – Utah
Utah’s big health care problem? It lacks hospital beds. Additionally, those that are in place are concentrated in the state’s one large metropolitan area, Salt Lake City.
Health Care in Utah
| Population | Hospital Beds (per 1k ppl) | Active Physicians (per 100k ppl) | Uninsured Residents |
|---|---|---|---|
| 3.206 million | 1.8 | 216.2 | 10.0% |
Beyond a lack of hospital beds, one out of every 10 Utahns doesn’t have health insurance at all, which doesn’t factor in the Utahns who are under-insured.
The University of Utah Medical School, featured in the video below, is making a concentrated effort to train more doctors in more critical care specialties and to expand medical care not only in Utah but also around the world.
Interestingly, residents of Utah have more term life insurance policies per capita than the residents of any other state in the United States (see the 10 Best and Worst States for Life Insurance). As Utah continues to grow and its population continues to become more diverse, we expect this bright spot to carry over into other health care markers.
#5 – Arizona
Across the board, Arizona has a low number of hospital beds and practicing doctors and a relatively high percentage of uninsured residents.
Health Care in Arizona
| Population | Hospital Beds (per 1k ppl) | Active Physicians (per 100k ppl) | Uninsured Residents |
|---|---|---|---|
| 7.279 million | 1.9 | 242 | 12.1% |
Additionally, only Utah spends less on its residents’ health care than the state of Arizona. While the U.S. average for health care expenditures per capita by state is $8,045 per year, Arizona spends just $6,452 a year.
Traditionally, Arizona has a strong anti-tax and anti-public spending spirit. But as demographics change — the state is becoming younger and less white — this spirit looks to be changing, too. As it changes, we believe more public money will go to the state’s health care systems and infrastructures.
Important: Arizona life insurance policies
#6 – Oklahoma
Oklahoma has the third least number of doctors per capita and the second most percentage of uninsured residents of any state in the United States.
Health Care in Oklahoma
| Population | Hospital Beds (per 1k ppl) | Active Physicians (per 100k ppl) | Uninsured Residents |
|---|---|---|---|
| 3.957 million | 2.8 | 206.7 | 16.5% |
Oklahoma has one of the largest Native American populations of any state In the country. Native American nations and tribes often have inadequate access to comprehensive medical care, as you can see in the CBS News video below.
Read more: Oklahoma Life Insurance
With higher than average rates of hypertension, diabetes, and heart disease, Native Americans are an especially vulnerable population at risk of suffering from the COVID-19 pandemic.
The Rural Health Care Information Hub provides some valuable and startling information on American Indian and Alaska Native populations (AI/AN). They explain that:
“Nonelderly AI/AN adults are more likely to be uninsured compared to nonelderly whites, 25% and 8% respectively, and that there are higher uninsured rates of AI/AN children (14%) compared to white children (4%).”
Additionally, for the last 15 years at least, federal funding for Native American health and wellness initiatives has been cut dramatically, leaving this already-vulnerable population even more at-risk during times such as the current COVID-19 crisis.
#7 – New Mexico
Like many of its Western neighbors, New Mexico is largely a rural state, which poses many medical care problems such as lack of accessible hospital beds or access to a practicing physician.
Health Care in New Mexico
| Population | Hospital Beds (per 1k ppl) | Active Physicians (per 100k ppl) | Uninsured Residents |
|---|---|---|---|
| 2.097 million | 1.8 | 244.8 | 11.0% |
New Mexican State Senator Pete Campos explains that:
“Months-long waits for medical appointments, hours-long drives to Albuquerque or across the state’s borders once appointments are made and the worsening shortage of health professionals throughout New Mexico are becoming routine and, sadly, expected.”
The Rural Health Information Hub reports that as of January 2020, New Mexico has only 10 critical access hospitals to serve over 2 million residents. Additionally, the state of New Mexico spends only $7,214 per year per resident on health care expenditures, well below the national average of $8,045.
Whether you live in a rural, suburban, or urban part of the state, you need to know about the New Mexico life insurance policies available to you and your family.
#8 – Georgia
The Peach State may be a surprising state to find on this list, given that it’s home to ultra-cosmopolitan Atlanta and a number of highly-respected institutions such as Emory University.
But the state has a very high percentage of uninsured residents, who are far more at risk to face severe health problems than their insured counterparts.
Health Care in Georgia
| Population | Hospital Beds (per 1k ppl) | Active Physicians (per 100k ppl) | Uninsured Residents |
|---|---|---|---|
| 10.62 million | 2.4 | 228.7 | 15.5% |
So why does Georgia have so many uninsured residents? In short: Georgia has a wide wealth gap that makes health insurance, sadly, an unaffordable luxury for many residents.
To illustrate this point, the state’s biggest population center, Atlanta, was recently declared the city with the largest income gap disparity in the United States, as you can see in the video below.
Read more about Georgia life insurance in our thorough guide.
#9 – South Carolina
South Carolina lacks hospital beds and active doctors, and has a pretty high rate of uninsured residents, as you can see in the table below.
Health Care in South Carolina
| Population | Hospital Beds (per 1k ppl) | Active Physicians (per 100k ppl) | Uninsured Residents |
|---|---|---|---|
| 5.149 million | 2.4 | 229.5 | 13.1% |
Like many of the states on this list, South Carolina faces a problematic urban-rural divide and has a much lower-than-average household income level, which means folks can afford less medical care to begin with.
State expenditures on public health care only worsen this problem. South Carolina spends only $7,311 per year per resident on health care, well below the national average of $8,045. The Kaiser Family Foundation reports that such public expenditures are a telling sign of overall health conditions in the state, which is itself a telling sign of how well or badly a state is prepared to face a viral pandemic.
Read more: South Carolina Life Insurance
#10 – North Carolina
Like its Carolinian neighbor to the south, North Carolina faces a lack of hospital beds and, despite having one of the finest medical schools at a public university in the country, a lack of practicing physicians.
Health Care in North Carolina
| Population | Hospital Beds (per 1k ppl) | Active Physicians (per 100k ppl) | Uninsured Residents |
|---|---|---|---|
| 10.49 million | 2.1 | 255 | 12.6% |
Also like many other states on this list, North Carolina has a large urban-rural divide. The state is attempting to address rural health care by building more state-of-the-art medical centers in rural areas of the state, like the one in the video below in Western North Carolina.
Medical schools like the one at the University of North Carolina-Chapel Hill play an important role in not only a state’s preparedness for a public health crisis but also research that benefits us all. Let’s take a look at the nation’s top medical research schools.
The 10 Best Medical Schools for Research
When it comes to battling public health pandemics such as the coronavirus, cutting-edge and reliable medical research is of the utmost importance. Treatments, vaccines, and other preventive measures come out of these institutions and help keep all of us safe.
As the Unite for Sight coalition explains, “The purpose of research is to inform action.”
So you might be wondering where the best medical schools for research are.
Every year, U.S. News & World Report ranks the best medical schools in the nation. They then break out these rankings into specialties, including research, but ranging from anesthesiology to pediatrics. For research, their ranking methodology is based on eight data indicators:
- Peer assessment score
- Assessment score by residency directors
- Research activity
- Total National Institutes of Health (NIH) research activity
- Average NIH research activity per faculty member
- Primary care rate
- Student selectivity
- Faculty resources
You can get a peek into student life at one of the consistently top-ranked research medical universities, Johns Hopkins University School of Medicine in Baltimore, in the video below.
Johns Hopkins has a unique pedagogical model, which helps lead to its top ranking in medical research. According to U.S. News:
“Students at the Johns Hopkins School of Medicine learn through the Genes to Society Curriculum, which pairs academics with concurrent clinical experience. Every few months, classes break for Intersessions, week-long special courses focused on simulation and advanced skills.”
No wonder doctors coming out of Johns Hopkins University School of Medicine are in such high demand: They come to the field already armed with the skills to fight pressing medical issues, both of the everyday and pandemic quality. And since medical school is expensive, it’s essential to investigate the unique insurance tips of college students and ways you can save on premiums.
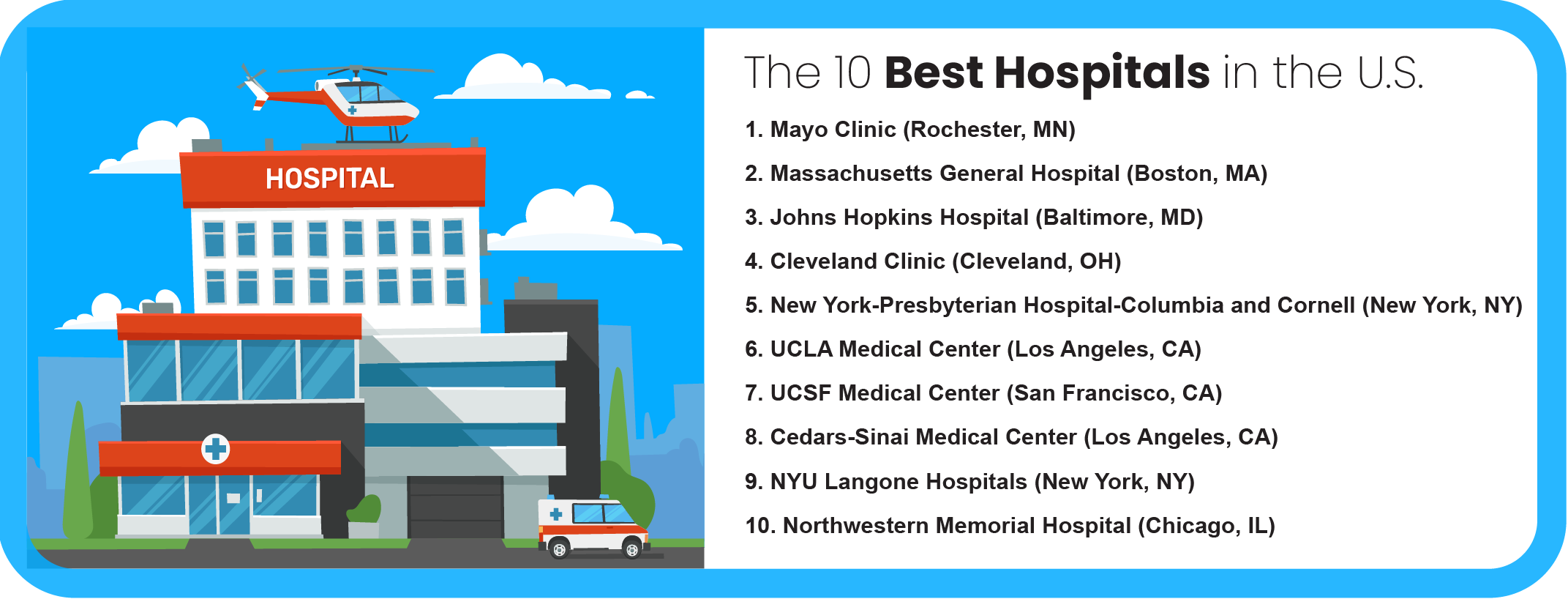
Now that we’ve taken a brief look at the top 10 medical schools for research, let’s round out our knowledge by taking a quick glance at the top 10 hospitals across the United States.
The 10 Best Hospitals in the United States
People love to go to the best places. Be it the best coffee shop or best auto mechanic, we’re always looking for the highest quality of service. When it comes to hospitals, our desire for the best is even more intense and important.
You’ll recognize the location of many of the 10 best hospitals as overlapping with the 10 states best prepared to face a pandemic. And many of them are connected to the best medical schools in the nation, as well.
So how does U.S. News & World Report come up with their yearly best hospital rankings?
Every year, the organization ranks 4,653 hospitals, which represent nearly all the inpatient medical centers across the United States. They explain that “the Best Hospitals Honor Roll is a ranked list of 20 hospitals that excelled in the 16 Best Hospitals specialties and nine procedures and conditions ratings.”
The nine procedures and conditions include the most common and critical types of surgery and treatments facing patients in the United States: colon cancer surgery, lung cancer surgery, heart bypass surgery, aortic valve surgery, abdominal aortic aneurysm repair, hip replacement, knee replacement, heart failure, and chronic obstructive pulmonary disease, or COPD.
But what about the 16 specialties that really shoot a hospital to the top of the Best Hospitals Honor Roll? In the table below, we’re providing those specialties and the top hospital for that specialty.
Best Hospitals by Specialty
| Specialty | Top Hospital | Hospital Location |
|---|---|---|
| Cancer | University of Texas MD Anderson Cancer Center | Houston, TX |
| Cardiology & Heart Surgery | Cleveland Clinic | Cleveland, OH |
| Diabetes & Endocrinology | Mayo Clinic | Rochester, MN |
| Ear, Nose, & Throat | Mayo Clinic | Rochester, MN |
| Gastroenterology & GI Surgery | Mayo Clinic | Rochester, MN |
| Geriatrics | Johns Hopkins Hospital | Baltimore, MD |
| Gynecology | Memorial Sloan-Kettering Cancer Center | New York, NY |
| Nephrology | Mayo Clinic | Rochester, MN |
| Neurology & Neurosurgery | Johns Hopkins Hospital | Baltimore, MD |
| Ophthalmology | University of Miami Hospital and Clinics–UHealth Tower | Miami, FL |
| Orthopedics | Hospital for Special Surgery | New York, NY |
| Psychiatry | Massachusetts General Hospital | Boston, MA |
| Pulmonology & Lung Surgery | National Jewish Health-Denver | Denver, CO |
| Rehabilitation | Shirley Ryan Ability Lab | Chicago, IL |
| Rheumatology | Johns Hopkins Hospital | Baltimore, MD |
| Urology | Mayo Clinic | Rochester, MN |
As you can see, the Mayo Clinic is not only the current top-ranked hospital overall but also the top-ranked in five of the 16 medical specialties. Located in Rochester, Minnesota, about an hour and a half southeast of Minneapolis, the Mayo Clinic brings in patients from all over the United States and around the world, especially during a crisis like COVID-19.
Sadly, life insurance is something we must think about during a time like the current coronavirus pandemic. This is also a really good time to consider the types of health insurance available to you and what each of them covers.
Your life insurance quotes are always free.
Secured with SHA-256 Encryption
Professionals Discuss Safety Prep & COVID-19
We asked a variety of reputable and relevant professionals to weigh in on the current and possible future state of public preparedness for the coronavirus and other possible pandemics in general.
Read on to find out some of the valuable and at times surprising insight they had to provide.
“There is a wide range of factors that affect the ability of a state to meet the challenges posed by this novel coronavirus.
Some states are better positioned than other states to meet the challenge of the pandemic based on the population density of the state. Those states that are operating with a less dense population will find less strain on critical infrastructure as compared with states that have a higher population density.
Urban areas such as New York have felt the strain of the pandemic most acutely especially in certain areas where the outbreak took hold early. The level of preparedness required of the state will be a much higher standard for states with a higher population density because the coronavirus is so infectious and transmits more rapidly in states with large cities and metropolis areas.
The ratio of physicians per resident of each state is another significant factor that will affect the level of preparedness required of a state.
The coronavirus pandemic has hit the elderly particularly hard. Those states with a higher population of seniors face more significant health care challenges. The level of preparedness required of these states will need to be much higher than in other states with younger populations.
It is also important to recognize that there is no state that was fully prepared for the arrival of the coronavirus, but some states have higher abilities to deal with the arrival then other states based on a higher degree of coordination with the private sector.
The level of preparedness of a state is measured by the ability of the state for not just health care needs but also the ability of the state to support commerce, keep facilities of education open, and maintain public safety. Those states with over-stretched budgets may find it harder to maintain essential services in the months ahead.
California, Texas, Michigan, and Washington have been least prepared for the arrival of the coronavirus based on current news reports. Other states such as West Virginia, Montana, and Vermont have not yet had the surge of cases as other states, but that may be due to the capacity to test for outbreaks.
Only after the pandemic is over in the future will we truly be able to accurately measure which state was best prepared.”
David Reischer, Esq., is the founder and CEO of LegalAdvice.com.
David is a licensed attorney with over 15 years of legal experience.
What states are best prepared to meet the Coronavirus pandemic head–on?
“States that are best prepared to meet the coronavirus pandemic head-on have made a concerted effort to update their healthcare systems and have implemented measures to prevent the spread of the virus.
These states have also invested in research and development to improve their ability to detect and respond to outbreaks quickly. States that are not as well prepared may struggle to keep up with the virus’s rapid spread.”
What states are least prepared to meet the Coronavirus pandemic head–on? Why?
“There are several reasons why some states are less prepared to meet the coronavirus pandemic head–on. One reason is that these states have not invested in the necessary infrastructure, such as laboratories and training centers.
Some states haven’t implemented policies or procedures to deal with a pandemic. Some state officials don’t believe a pandemic is happening. Many factors contribute to state preparedness for a pandemic. By doing so, all residents will be protected.”
What makes a state prepared for a pandemic?
“A state is prepared for a pandemic when it has a well-organized health system, reliable communication systems, and enough resources to support the population. To be ready, a state must have a plan for the virus and a strategy for managing the influx of patients and resources. A state must also have resources to enforce quarantine measures and track potential carriers.”
What measures are you seeing in your state, city, or region to combat the pandemic?
“Many states, cities, and regions are taking measures to combat the pandemic. Some institute mandatory quarantines for people infected with the pandemic virus, while others restrict access to public transportation and schools.
Some hospitals have instituted restrictions on visitors, and some businesses have closed. There is no one answer to this question; each community will decide what measures they need to protect themselves from the pandemic.”

Dr. Amir Majidi is the CEO of StudioAthletica.com.
Amir is a board-certified doctor who treats musculoskeletal injuries.
What states are best prepared to meet the Coronavirus pandemic head–on?
“The United States is facing a potentially devastating public health crisis from the Coronavirus pandemic. The virus originated in China and has spread throughout the world and has now reached the U.S. As of this writing, there are over 1,000 confirmed cases of the Coronavirus in the United States and over 30 deaths.
The states that are best prepared to meet the Coronavirus pandemic head-on have been preparing for such an event for years. These states have implemented robust public health infrastructure and policies to protect their citizens from infectious diseases. They also have strong partnerships with hospitals and other healthcare providers, enabling them to respond rapidly to outbreaks.
Some of the best-prepared states include California, New York, Washington, and Oregon. These states have been leaders in implementing policies and programs to prevent and control the spread of infectious diseases. For example, California has a statewide system for tracking and responding to infectious disease outbreaks, which includes a network of surveillance sites across the state.
New York has a similar system in place and a state law requiring all hospitals to report cases of certain communicable diseases to the state Department of Health.
Both Washington and Oregon have implemented policies that require hospitals to report cases of certain infectious diseases to public health authorities. In addition, both states have laws that allow for the quarantine of individuals who are suspected of having an infectious disease.”
What states are least prepared to meet the Coronavirus pandemic head–on? Why?
“The United States is facing a potentially severe outbreak of the Coronavirus, and some states are better prepared than others to meet the challenge.
The states least prepared to deal with the outbreak are those that have been hit hardest by the recent flu season and those with large populations of vulnerable people, such as the elderly or those with chronic health conditions. These states include California, Texas, Florida, and New York.
The states mentioned above have been stretched thin by the flu, which has overwhelmed hospitals and other medical facilities. They also have many people at high risk for serious complications from the virus, such as the elderly or those with chronic health conditions.
These states have large international airports, which increases the chances that the virus will spread there. The good news is that all of these states are taking steps to prepare for the possibility of a coronavirus outbreak. However, it remains to be seen whether they can effectively contain the virus if it does begin to spread widely.”

Stephanie Edenburgh is the CEO of BizzieMommy.com.
Her site provides advice to families regarding health, safety, and more.
What States are best & least prepared for the Coronavirus pandemic?
“The United States is facing a potentially devastating pandemic, and some states are far better prepared than others.
According to a new report from the Trust for America’s Health, Massachusetts, Rhode Island, and Connecticut are the best-prepared states in the country, while Alaska, Louisiana, and Oklahoma are the least prepared.
The report rates states on various factors, including public health funding, disease surveillance, and emergency preparedness. It also examines whether states have implemented key recommendations from the Centers for Disease Control and Prevention (CDC).
Massachusetts, Rhode Island, and Connecticut all received high marks for public health funding, disease surveillance, and emergency preparedness. They also have implemented key CDC recommendations, such as expanding access to vaccinations and increasing lab capacity.
On the other hand, Alaska, Louisiana, and Oklahoma received low marks for public health funding and disease surveillance. They also still need to implement vital CDC recommendations.(For more information, read our “Louisiana Life Insurance“).
This is a dire situation, and states must take steps to protect their residents. The Trust for America’s Health report is a valuable resource for states to assess their preparedness levels and take action.”
What measures are you seeing in your state, city, or region to combat the pandemic?
“The first step that many states and cities are taking is to close non–essential businesses. This includes things like gyms, movie theaters, and malls. Restaurants are also closing their dining rooms and switching to take–out or delivery only. Schools are closed for the foreseeable future, with some districts moving to online learning. Governors are also implementing strict travel restrictions.
For example, New York requires a 14–day quarantine for anyone coming from out of state. And in California, all non–essential travel is discouraged. Hospitals are preparing for an influx of patients by increasing ICU capacity and stockpiling supplies.
Healthcare workers are trained to use personal protective equipment (PPE) correctly. These are just a few of the measures being taken to combat the pandemic. Every state, city, and region does something slightly different depending on its needs. But the goal is always the same: to slow the spread of the virus and keep people healthy and safe.”

Jaqueline Miranda is a research assistant for PracticalPsychology.com.
This company provides guides and resources for psychology and mental illness.
What states are best prepared to meet the coronavirus pandemic head-on?
“The states that are best prepared for coronavirus are those with tight-knit local communities who are ready to adapt to extenuating circumstances such as a pandemic.”
What states are least prepared to meet the coronavirus pandemic head-on? Why?
“It’s important to recognize that coronavirus, like most other infectious diseases, impacts densely populated metropolitans and cities more than anywhere else.”
As a result, these localities must do more to prepare than their rural counterparts. More care and concern are required for states with such areas.
What makes a state prepared for a pandemic?
“Knowing how to respond to the needs of individuals and businesses is a must if a state wants to be prepared for a pandemic. Implementing safety precautions and preventing the spread of the illness is fairly straightforward. Especially when following CDC guidelines.
Therefore, for a state to be effectively prepared for a pandemic, it must have avenues for individual and community-level groups to address and mitigate their concerns.
By their very nature, governments, both state and federal, are very large entities that can quickly make sweeping orders that affect the population as a whole. But they are incapable of meeting the needs of the individual because they have to focus on the safety of the community at large.
As a result, state governments may fail to recognize the real-life implications such orders may have on individuals’ daily life —such as feeding their family, maintaining their home, or paying their bills on time in order to keep some semblance of natural order.
All in all, in order for a state to be prepared for a pandemic, it must be ready to not only prevent the spread of disease. But also have established networks to support the communities, and thus, individuals. Either by working with city, county, and local governments, or community organizations.”
What measures are you seeing in your state, city, or region to combat the pandemic?
“There are lots of measures being taken by the general public in North Carolina in order to prevent the spread of disease.
I have seen plexiglass at checkouts in stores, ‘one-way’ shopping aisles, tape in the grocery stores to designate appropriate social distancing. The general public has been wearing masks and gloves as well.”
Douglas Dedrick is the founder and lead researcher of HealingLaw.com.
His organization is dedicated to making U.S. laws easy to understand for all.
“No state is particularly well suited to meet the coronavirus pandemic head-on for many reasons.
The main reason is that people stop working and hunker down on their economic activity, which causes sales and income taxes to drop. This will eventually shrink property taxes.
Since states can’t borrow as cheaply as the federal government and have balanced budget amendments, that forces them to raise taxes or cut spending in other areas to pay for personal protective equipment, ventilators, and meet other demands right now as well go through this crisis.
Once each state’s budget year ends and they take a look at their revenue shortfalls, they’re going to have to make even more draconian cuts and tax increases to maintain their budgets, further depressing the economy.
States would be better prepared for pandemics if they had good rainy day funds to tap into during crises such as the one we are in today. States should be able to transfer resources to where they’re most needed faster during times like these.
The states least prepared for fighting a pandemic are the ones with the biggest budget deficits, which are likely the ones most dependent on the price of oil for their public revenues like North Dakota, Alaska, and Texas.
Read more: North Dakota Life Insurance
Smaller oil-rich states like Alaska and Wyoming don’t have as many cases as bigger states like Michigan or New York, but they will still struggle to meet their needs due to falling severance taxes. Some of these states don’t have income or sales taxes at all but are still likely to see massive shortfalls.
One way that states could be better prepared for pandemics would be to pass their own state-level versions of the Defense Production Act. This would allow governors to order private companies to produce what is necessary during emergencies when the federal government refuses to intervene or support them.”
Casey Adams, with Hudson Wealth Management, specializes in insurance.
He is also a grad student studying to obtain a public administration degree.
Frequently Asked Questions
Is COVID-19 going away?
Although the coronavirus seemed to abate a little over the summer, reports from different countries are suggesting that there are new spikes in cases, with governments facing pressure to either lockdown their country again or risk widespread contagion and death.
Should I get tested if I had close contact with someone who has COVID-19?
If you have had close contact with someone who has COVID-19, the CDC recommends that you consult with your doctor to determine if you need a test. In general, a person who has had close contact with a person who tested positive for COVID-19 should self-quarantine for 14 days and watch for coronavirus symptoms.
When was the COVID-19 pandemic declared?
The World Health Organization declared COVID-19 a pandemic on March 11, 2020. This came during a time when a number of countries were experiencing a spike in cases and shortly before the cases outside of China grew larger than the cases inside China.
Can I stay at home if I have presumed COVID-19?
If you have presumed COVID-19, the general rule is to isolate or self-quarantine at home, only leaving your house for medical treatment. This will reduce the possibility of you spreading the disease to the larger community.
Can you contract the coronavirus disease from a package in the mail?
The CDC says there is no evidence that someone can contract the coronvirus disease from a package in the mail. Although the coronavirus can remain on surfaces for a number of hours, this is not its primary method of transmission. It predominantly spreads through direct person-to-person contact and respitarory droplets.
Does the CDC recommend the use of masks to reduce spread of COVID-19?
Yes, the CDC recommends the use of masks to reduce the spread of the novel coronavirus. It specifically recommends wearing them when using public transportation or during gatherings involving a large number of people.
Is there a vaccine for the coronavirus disease?
As of this writing, no, however certain vaccines are reaching the last stages of testing with some showing a positive effect in the fight against COVID-19. One of the main issues with the vaccines are the possible side effects they’ll have on patients or the general public.
Your life insurance quotes are always free.
Secured with SHA-256 Encryption
Laura D. Adams
Insurance & Finance Analyst
Laura Adams is one of the nation’s leading finance, insurance, and small business authorities. As an award-winning author, spokesperson, and host of the top-rated Money Girl podcast since 2008, millions of readers and listeners benefit from her practical advice. Her mission is to empower consumers to live healthy and rich lives by planning for the future and making smart money decisions. She rec...
Insurance & Finance Analyst
Editorial Guidelines: We are a free online resource for anyone interested in learning more about life insurance. Our goal is to be an objective, third-party resource for everything life insurance-related. We update our site regularly, and all content is reviewed by life insurance experts.